Cardbio pt
From 2013.igem.org
Contents |
The Problem
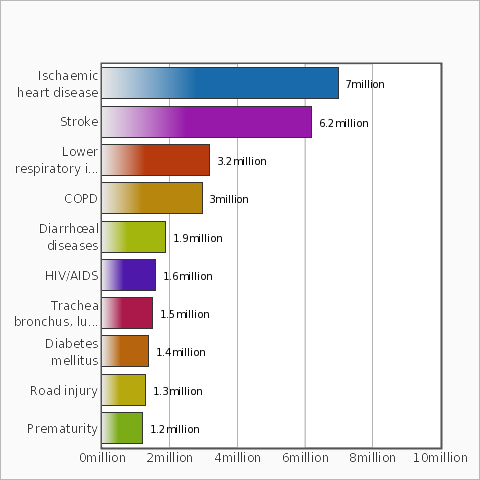
Acute coronary syndrome (ACS) refers to any group of clinical symptoms compatible with acute myocardial ischemia and includes unstable angina, non—ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction (Kumar and Cannon, 2009). These high-risk manifestations of coronary atherosclerosis are important causes of the use of emergency medical care and hospitalization in the United States, where in 2004, approximately 200.000 people died by heart attack, and in 2009, about 1.190.000 patients were diagnosed with ACS (Acute Coronary Syndrome) (Heart Disease and Stroke Statistics--2012 Update : A Report From the American Heart Association). According to World Health Organization report, ischemic heart disease and stroke are the leading causes of death in the world leading to 13.2 million deaths in 2011.
The high number of death in ACS is deeply related to its late diagnosis, which is usually made after the cardiac event had already occurred. It is observed in ACS that plaque formation and its development release several substances in the patient blood that have a big potential to be explored as possible biomarkers for diagnosis of ACS. In this context, several biomarkers are described to pathophysiological processes associated with acute myocardial infarction as shown in the Figure 2.

Given the importance of this pathophysiological processes, Brazil_UFMG team chose to develop a Genetically Modified Organism able to measure blood serum concentrations of 3 specific ACS biomarkers as a potential prognostic test for this syndrome.
References:
- Kumar A., Cannon, C. P.,(2009) ”Acute Coronary Syndromes: Diagnosis and Management, Part I” Mayo Clinic Proceedings, vol 84, Issue 10, pages 917–938 Symposium on Cardiovascular Diseases.
- Danne, O. and Möckel, M. (2010). "Choline in acute coronary syndrome: an emerging biomarker with implications for the integrated assessment of plaque vulnerability." Expert Rev Mol Diagn 10(2): pages 159-171.
- Heart Disease and Stroke Statistics - 2012 Update : A Report From the American Heart Association.
- Searle J, Danne O, Müller C, Mockel M.(2011). "Biomarkers in acute coronary syndrome and percutaneous coronary intervention." Minerva Cardioangiol.
- Chan, D. and Ng L. L., “Biomarkers in acute myocardial infarction”, BMC Med. 2010; 8: 34. Published online 2010 June 7
- “The top 10 causes of death“, World Health Organization, July 2013, http://www.who.int/mediacentre/factsheets/fs310/en/index.html
CardBio: The Project
Death by heart diseases is very common worldwide, being Acute Coronary Syndrome (ACS) its main cause. This fact is deeply related to late diagnosis, which is usually made after the cardiac event had already occurred. We, from UFMG team, decided to explore this problem building a system capable of providing a precocious diagnosis for ACS based in 3 biomarkers: Brain Natriuretic Peptide (BNP), Trimethylamine-N-Oxide (TMAO) and Ischemia Modified Albumin (IMA). The main goal is to detect each of these biomarkers using our engineered E. coli by integrating the signals CFP, YFP and RFP produced when BNP, IMA and TMAO, respectively, are present in a sample of patient serum. This diagnosis is based on color intensity of the fluorescent proteins. So, we can establish the presence or absence and severity of ACS disease and predict earlier a myocardial event, thus providing information for fast treatment.
Our Design
After an extensive research on the biomarkers used for prognosis of Acute Coronary Syndrome (ACS), we elected three that we could work on to somehow make our bacteria detect: IMA, TMAO and BNP.
IMA, which means Ischemia Modified Albumin, was a tricky one. Literature indicated that, although a good marker for ischemia, IMA could be better used as a negative predictor for ACS prognosis. Because of that, we developed a system to use the expression of YFP in E. coli as a warning that IMA is increasing, in which the absence of yellow fluorescence means that everything is still ok. Since IMA is known to have lower capacity to bind cobalt than normal human serum albumin, a clinical test based on the detection of cobalt added to a patient’s blood serum is available; therefore, we decided to incorporate this method in our bacterial system by using a cobalt-inducible promoter, Rcna (BBa_K540001), associated with the YFP translational unit (BBa_E0430). Bacteria carrying this plasmid construction growing in medium containing cobalt should express high levels of YFP, which can be easily detected by fluorimetric methods. However, if we add normal serum, the albumin should bind the cobalt resulting in lower fluorescence. Thus, the presence of IMA in sera from ACS patients could be detected by measuring YFP expression: in the presence of IMA, cobalt remains in its free form and, through the activation of the co-inducible promoter, the bacteria will express YFP.
TMAO is a biomarker that was recently linked to heart diseases, and one that our research literature showed that could activate an inducible bacterial promoter, part of the TorCAD operon. Since this promoter was not deposited in the Parts Registry, we ordered it to be synthesized, with modifications to its structure to enhance its activity [1]. The sequence of the promoter we ordered was:
5’ – CGAACGAATTCGCGGCCGCTTCTAGAGATTCTGTTCATATCTGTTCATATTCCGTTCATCCT
GACCAGTGCCGCTGTTCATATTTGCTCATTAAGATCGCTTCATACTAGTAGCGGCCGCTGCAG – 3’
We selected RFP as a reporter to detect this biomarker, and thus our construction for this device became the TorCAD promoter we had synthesized followed by the RFP translational unit (BBa_J06702).
Our last target is BNP (Brain Natriuretic Peptide), a major prognostic biomarker for ACS. To detect it, we tried to synthesize a biobrick containing the coding region of NPRA, a receptor capable of detecting BNP and respond unleashing an intracellular cGMP cascade. And to detect the cGMP produced by the receptor, we also ordered the synthesis of another promoter, belonging to PDE5 (phosphodiesterase 5), which is positively regulated by this molecule. Putting it all together, the plan was to create a plasmid containing two constructions: 1) a constitutive promoter associated with the translational unit of NPRA, to make our bacteria detect BNP and respond producing cGMP, and 2) PDE5 promoter associated with the translational unit of another fluorescent protein, like CFP, to make our bacteria produce a signal when the biomarker was detected. However, we were unable to proceed with the detection of BNP, due to the high content of CG pairs on both the NPRA receptor and PDE5 promoter, which rendered their synthesis impossible.
Thus, by inserting all of these inside our Escherichia coli, we’d have in our hands our heart vigilant bacteria, ready to save some lives!

References:
- Ansaldi M, Simon G, Lepelletier M, Mejean V (2000). "The TorR high-affinity binding site plays a key role in both torR autoregulation and torCAD operon expression in Escherichia coli." J Bacteriol 2000;182(4);961-6. PMID: 10648521
Biomarkers
TMAO
Trimethylamine N-oxide (TMAO) is a relatively common diet metabolite in animals. It originates from the degradation of choline, present in the phosphatidylcholine (lecithin) from foods like eggs, milk, liver, red meat, poultry, shellfish and fish. Choline and other trimethylamine-containing species (for example, betaine) are degraded by intestinal microbes, forming the gas trimethylamine (TMA). This molecule is then absorbed and metabolized in the liver by flavin monooxygenases (FMO), forming TMAO (Wang et al., 2011).
A study published in 2013 (Tang et al., 2013) associated TMAO levels in blood with heart disease, and pointed that gut flora has an important role in forming this molecule in humans. The demonstrated relationship between TMAO levels and future cardiac events like heart attack, stroke, and death could be established even in cases with no prior evidence of cardiac disease shown by the traditional methods.
TMAO also alters cholesterol deposition and removal from endothelial cells. Dietary TMAO aggravate the development of atherosclerotic lesions in apolipoprotein E null (apoE−/−) mice without significant alterations in plasma cholesterol, triglycerides, lipoproteins, glucose levels, and hepatic triglyceride content. But the precise molecular mechanisms in which TMAO mediates its proatherosclerotic effect are currently unknown (Koeth et al., 2013). Given this evidence, TMAO could act as good biomarker for prognosis of cardiovascular risk, although more studies are still needed to validate TMAO testing as clinical tool for preventing cardiovascular diseases.
With the aim of developing an innovative prognostic test for acute coronary syndrome, The Cardbio project included TMAO detection. This biomarker emerged in recent, good quality and strong evidence-based research and seems like a good candidate for early detection of atherosclerotic plaque formation.
References
- Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013 Apr 25;368(17):1575-84. doi: 10.1056/NEJMoa1109400.
- Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, Smith JD, DiDonato JA, Chen J, Li H, Wu GD, Lewis JD, Warrier M, Brown JM, Krauss RM, Tang WH, Bushman FD, Lusis AJ, Hazen SL.Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013 May;19(5):576-85. doi: 10.1038/nm.3145. Epub 2013 Apr 7.
- Bennett BJ, de Aguiar Vallim TQ, Wang Z, Shih DM, Meng Y, Gregory J, Allayee H, Lee R, Graham M, Crooke R, Edwards PA, Hazen SL, Lusis AJ. Trimethylamine-N-oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab. 2013 Jan 8;17(1):49-60. doi: 10.1016/j.cmet.2012.12.011.
- Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS,Dugar B, Feldstein AE, Britt EB, Fu X, Chung YM, Wu Y, Schauer P, Smith JD, Allayee H, Tang WH, DiDonato JA, Lusis AJ, Hazen SL. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011 Apr 7;472(7341):57-63. doi: 10.1038/nature09922.
- Mayr M. Recent Highlights of Metabolomics in Cardiovascular Research. Circulation: Cardiovascular Genetics. 2011; 4: 463-464
IMA
One of the main aspects of acute coronary syndrome is myocardial ischemia. It occurs when blood flow to heart muscle is decreased by a partial or complete blockage of coronary arteries, reducing oxygen supply. If the ischemia is detected early, it can be reversed with no myocardial permanent impairement. However, if it is prolonged, there will be cellular necrosis and myocardial infarction. Currently, the only strategy for detecting ischemia is to detect ST segment changes on the electrocardiogram (ECG) but with only around 50% sensitivity. There is, therefore, a need for an early diagnosis for myocardial ischemia so it can be treated in time.
Serum albumin is the most abundant protein in human blood. It is responsible for binding, transporting and distributing a number of small molecules and metallic ions, such as Fe2+, Ni2+, Cd2+ e Co2+. Studies conducted by Bar-Or et al., revealed that albumin extracted from patients with ischemia in cardiac tissues presented reduced cobalt binding. This reduction is probably due to the loss of two aminoacids in the albumin N-terminal – Asp1 e Ala2 – which constitutes an important binding site for metals in the protein (Sadler et al., 1994) and are known for being particularly susceptible to degradation, comparing to other N-terminal residues in other species (Chan et al., 1995). Recent studies (Oh et al., 2012; Lu et al., 2012) suggests, however, that the reduced albumin affinity for cobalt occurs not by the N-terminal damage, but by the binding of free fatty acids, which are increased in ischemic cases (Apple et al., 2004), in this portion of the protein, obstructing the cobalt binding site. Therefore, IMA detection could be a measure of free fatty acids in blood, which have been recently pointed as good biomarkers for prognosis of acute coronary syndrome (Breitling et al., 2011).
A colorimetric test for ischemia modified albumin (IMA) was developed (Bar-Or et al., 2000), based on the measure of free cobalt after the addition of patient sera with ischemia suspicion. Studies comparing the clinical use of this cobalt binding assay (CBA) with other biomarkers point to a high sensibility for ischemia detection, but with low specificity (Bhagavan et al., 2003; Christenson et al., 2001). This assay has a high negative predictive value and can be used in initial triage in clinic, and was approved by FDA (Foods and Drugs Administration) for detection/exclusion of acute myocardial infarction in 2003. Therefore, the Cardbio project chose IMA as a biomarker to be detected by its construction. Associated with other more specific biomarkers, IMA detection can improve the sensibility of our test and it also accomplishes our goal to detect the early alterations caused by acute coronary syndrome instead of diagnosing late events that cannot be reversed.
References
- Bar–Or D, Lau E, Rao N, Bampos N, Winkler JV, Curtis CG. Reduction in the cobalt binding capacity of human albumin with myocardial ischemia. Ann Emerg Med 1999;34(4 Suppl):S56.
- Bar–Or D, Lau E, Rao N, Bampos N, Winkler JV, Curtis CG. Characterization of the Co2+ and Ni2+ binding amino-acid residues of the N-terminus of human albumin. Eur J Biochem 2001;268:42-7
- Sadler PJ, Tucker A, Viles JH. Involvement of a lysine residue in the N-terminal Ni21 and u21 binding site of serum albumins. Comparison with Co21, Cd21, Al31. Eur J Biochem 1994;220:193–200.
- Chan B, Dodsworth N, Woodrow J, Tucker A, Harris R. Site-specific N-terminal auto-degradation of human serum albumin. Eur J Biochem 1995;227:524–8.
- Bar-Or, D., Lau, E. & Winkler, J.V. (2000) A novel assay for cobalt-albumin binding and its potential as a marker for myocardial ischemia - a preliminary report. J. Emerg Med. 19,311-315.
- Bhagavan, N. V.; Lai, E. M.; Rios, P. A.; Yang, J. S.; Ortega-Lopez, A. M.; Shinoda, H.; Honda, S. A. A.; Rios, C. N.; Sugiyama, C. E.; Ha, C. E. Evaluation of human serum albumin cobalt binding assay for the assessment of myocardial ischemia and myocardial infarction. Clin. Chem. 2003, 49, 581−585.
- Christenson, R. H.; Duh, S. H.; Sanhai, W. R.; Wu, A. H. B.; Holtman, V.; Painter, P.; Branham, E.; Apple, F. S.; Murakami, M.; Morris, D. L. Characteristics of an albumin cobalt binding test for assessment of acute coronary syndrome patients: A multicentre study. Clin. Chem. 2001, 47, 464−470.
- Oh BJ, Seo MH, Kim HS. Insignificant role of the N-terminal cobalt-binding site of albumin in the assessment of acute coronary syndrome: discrepancy between the albumin cobalt-binding assay and N-terminal-targeted immunoassay. Biomarkers. 2012 Aug;17(5):394-401
- Lu J, Stewart AJ, Sadler PJ, Pinheiro TJ, Blindauer CA. Allosteric inhibition of cobalt binding to albumin by fatty acids: implications for the detection of myocardialischemia. J Med Chem. 2012 May 10;55(9):4425-30
- Apple, F. S.; Kleinfeld, A. M.; Adams, J., III. Unbound free fatty acid concentrations are increased in cardiac ischemia. Clin. Proteomics J. 2004, 1, 41−44.
- Breitling, L. P.; Rothenbacher, D.; Grandi, N. C.; Marz, W.; Brenner, H. Prognostic usefulness of free fatty acids in patients with stable coronary heart disease. Am. J. Cardiol. 2011, 108, 508−513.
- David C. Gaze. Ischemia Modified Albumin: A Novel Biomarker for the Detection of Cardiac Ischemia. Drug Metab. Pharmacokinet. 24 (4): 333–341 (2009).
BNP
BNP (Brain Natriuretic Peptide) is synthesized mainly by the ventricles, and their circulatory concentrations are significantly elevated in congestive heart failure (CHF).
The plasma concentration of BNP has been used to assist in the accurate diagnosis of heart failure in patients admitted with symptoms of decompensated heart failure (Abassi et al., 2004).
In humans, BNP is produced from proBNP, which contains 108 amino acids and, after proteolytic processing, releases a mature molecule and a 32 aminoacid N-terminal fragment in the circulation. BNP was originally cloned from brain but is now considered a blood hormone produced mainly in the heart ventricles (Ogawa et al. 1991). It is now known that these peptides have effects such as diuresis, natriuresis, vasodilation, and act as a circulating hormone in the inhibition of aldosterone synthesis and renin secretion. Thus, BNPs seems to play an important role in the regulation of blood pressure and blood volume (Nishikimi et al., 2006).
BNP is released by injured heart in very expressive proportions. Therefore, physicians have become very interested in measuring the plasma levels of BNP as a diagnostic tool in cardiology. In fact, several studies have shown that the measurement of circulating BNP can discriminate between patients with decompensated congestive heart failure and patients with dyspnea due to noncardiac etiology (Lemos et al., 2001). Evaluation of BNP levels should not be used as an independent test, but its high sensitivity and negative predictive value may be useful to add other information to the physician in making a diagnosis of heart failure. The main strength of BNP is the excellent negative predictive value with regard to left ventricular dysfunction and heart failure, but other specific diagnostic tools are required to define the actual abnormality (Vuolteenaho et al., 2005).
The Cardbio project chose to use BNP in its construction because it is a biomarker already used with diagnostic purposes, with several commercial assays already developed for its quantitative immunodetection. These assays could be used as controls, to validate our construction. In addition to this, since BNP is a small, unstable molecule that can be underestimated by immunoassays relying on antibody recognition (Tamm et al., 2008), a synthetic biology approach could improve the heart failure diagnosis based on this biomarker.
References
- Vuolteenaho O, Ala-Kopsala M, Ruskoaho H. BNP as a biomarker in heart disease. Adv Clin Chem. 2005;40:1-36.
- Lemos, J. A., Morrow, D. A., Bentley, J. H., Omland, T., Sabatine, M. S., McCabe, C. H., Hall, C., Cannon, C. P., & Braunwald, E. (2001). “The prognosis value of B-type natriuretic peptide in patients with acute coronary syndromes.” N Engl J Med 345, 1014–1021.
- Toshio Nishikimi, Nobuyo Maeda, Hiroaki Matsuoka (2006). “The role of natriuretic peptides in cardioprotection.” Elsevier Cardiovascular Research 69 (2006) 318 – 328
- Zaid Abassi, Tony Karram, Samer Ellaham, Joseph Winaver, Aaron Hoffman (2004).”Implications of the natriuretic peptide system in the pathogenesis of heart failure: diagnostic and therapeutic importance.” Elsevier Pharmacology & Therapeutics 102 (2004) 223– 241
- Natalia N. Tamm, Karina R. Seferian, Alexander G. Semenov, Kadriya S. Mukharyamova, Ekaterina V. Koshkina, Mihail I. Krasnoselsky, Alexander B. Postnikov, Daria V. Serebryanaya, Fred S. Apple, MaryAnn M. Murakami, and Alexey G. Katrukha. Novel Immunoassay for Quantification of Brain Natriuretic Peptide and Its Precursor in Human Blood. Clinical Chemistry 54:9 1511–1518 (2008)
Our Sponsors


 "
"